Platelets (Thrombocytes)
Platelets, also known as thrombocytes, are tiny blood cells that play a crucial role in blood clotting and wound healing.
Immune Thrombocytopenia (ITP):
This condition is characterized by a low platelet count due to the immune system mistakenly attacking and destroying platelets. As a result, individuals with ITP may experience an increased risk of bleeding and bruising.
Thrombocytopenia: Low Platelet Count
Thrombocytopenia refers to a low platelet count in the blood, which can result from various causes. The primary causes can be broadly categorized into decreased platelet production, increased platelet destruction, and sequestration.
Decreased Platelet Production
Bone Marrow Disorders:
- Aplastic Anemia: Bone marrow fails to produce sufficient blood cells.
- Leukemia: A type of cancer affecting blood and bone marrow.
- Myelodysplastic Syndromes: A group of disorders caused by poorly formed or dysfunctional blood cells.
- Bone Marrow Infiltration: Cancer or infections can infiltrate the bone marrow, reducing its ability to produce platelets.
Nutritional Deficiencies:
- Vitamin B12 Deficiency: Can lead to a reduction in platelet production.
- Folate Deficiency: Another vital nutrient whose deficiency can cause low platelet count.
Congenital Disorders:
- Fanconi Anemia: A rare genetic disorder affecting bone marrow.
- Congenital Amegakaryocytic Thrombocytopenia: A genetic condition leading to low platelet production.
- Thrombocytopenia with Absent Radius (TAR) Syndrome: A rare genetic disorder with low platelet count and absent radius bone in the forearm.
Infections:
- Viral Infections: Such as Epstein-Barr virus, cytomegalovirus, and HIV can decrease platelet production.
Increased Platelet Destruction
Immune-Mediated:
- Immune Thrombocytopenic Purpura (ITP): An autoimmune disorder where the body attacks its platelets.
- Drug-Induced Thrombocytopenia: Medications like heparin and quinine can cause this condition.
- Post-Transfusion Purpura: A rare complication following blood transfusion.
Non-Immune-Mediated:
- Disseminated Intravascular Coagulation (DIC): A serious disorder causing widespread clotting and bleeding.
- Thrombotic Thrombocytopenic Purpura (TTP): A condition causing small blood clots throughout the body.
- Hemolytic Uremic Syndrome (HUS): Often triggered by infection, leading to blood clot formation.
Infections:
- Bacterial Sepsis: Severe infection spreading through the blood.
- Viral Infections: Such as dengue fever, can also lead to increased platelet destruction.
Sequestration
Hypersplenism:
- Splenomegaly: Enlarged spleen due to liver disease or hematologic disorders can trap and reduce the number of platelets in circulation.
Thrombocytosis: High Platelet Count
Thrombocytosis is characterized by an elevated platelet count and can be divided into primary (essential or hereditary) and secondary (reactive) types.
Primary Thrombocytosis
Essential Thrombocythemia:
- A rare disorder causing increased platelet production due to clonal expansion of hematopoietic stem cells.
Hereditary Thrombocytosis:
- Genetic mutations (e.g., in the THPO or MPL genes) lead to increased platelet production.
Secondary (Reactive) Thrombocytosis
Infections:
- Bacterial, viral, or fungal infections can trigger elevated platelet counts as part of an acute phase response.
Inflammatory Conditions:
- Chronic diseases like juvenile rheumatoid arthritis, inflammatory bowel disease, and Kawasaki disease.
Tissue Damage:
- Trauma, surgery, or burns can increase platelet counts as part of the healing process.
Iron Deficiency:
- A common cause of reactive thrombocytosis in children.
Post-Splenectomy:
- Removal of the spleen can lead to persistently elevated platelet counts.
Hemolytic Anemia:
- Conditions causing hemolysis, such as sickle cell disease, can increase platelet production.
Medications:
- Drugs like corticosteroids can elevate platelet counts.
Malignancies:
- Some cancers, especially those affecting bone marrow, can cause elevated platelet production.
Chronic Blood Loss:
- Chronic conditions causing blood loss can stimulate platelet production as a compensatory mechanism.
Understanding Immune Thrombocytopenic Purpura (ITP)
Immune Thrombocytopenic Purpura (ITP) is an autoimmune disorder where the immune system mistakenly attacks and destroys platelets, leading to low platelet counts, bleeding, and bruising.
Overview
- Definition: ITP involves the immune system producing antibodies against platelets.
- Prevalence: It is relatively common in children, with about 1 in 10,000 affected each year.
Causes
- Autoimmune Reaction: The exact cause is often unknown, but it involves antibody production against platelets.
- Triggers: Infections (e.g., viral illnesses like measles, mumps, flu), vaccinations, or other immune challenges.
Symptoms
- Bruising: Easy or excessive bruising without a known cause.
- Petechiae: Small red or purple spots on the skin.
- Nosebleeds and Bleeding Gums: Particularly after brushing teeth.
- Heavy Menstrual Bleeding: In adolescent girls.
- Severe Bleeding: Rarely, severe internal bleeding can occur.
Diagnosis
- History and Physical Examination: Reviewing recent illnesses or vaccinations and examining signs of bleeding.
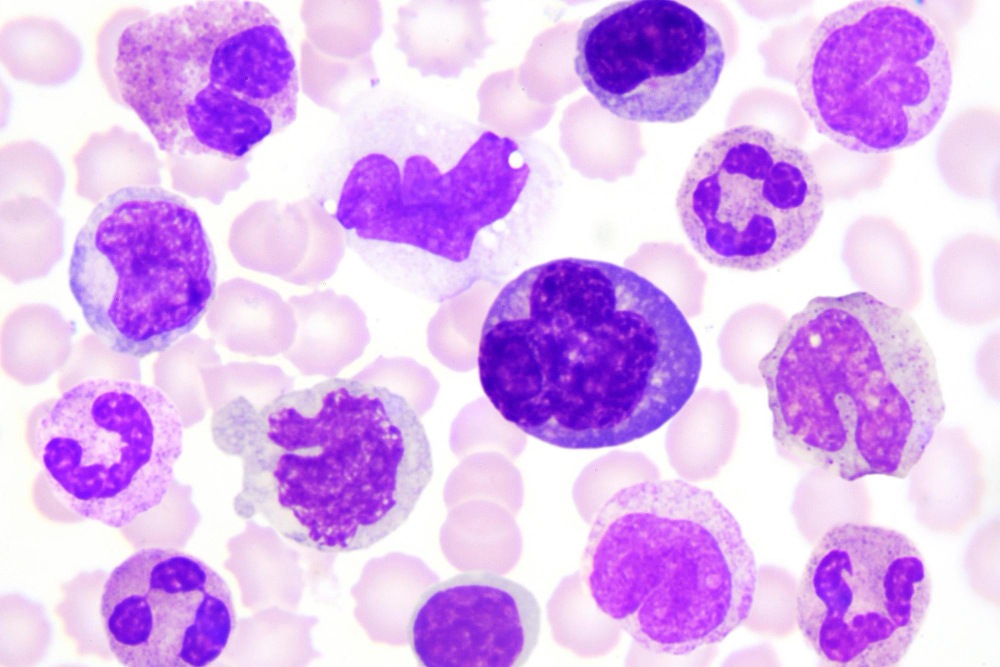
- Blood Tests: Complete blood count showing low platelet count and peripheral blood smear.
- Bone Marrow Exam: Rarely needed but can exclude other bone marrow disorders.
Treatment
- Observation: Many mild cases resolve on their own.
- Medications: Corticosteroids, intravenous immunoglobulin (IVIG), and anti-D immunoglobulin for Rh-positive children.
- Chronic ITP: Additional treatments include Rituximab, thrombopoietin receptor agonists, and possibly splenectomy.
Prognosis and Management
- Acute ITP: Most children recover spontaneously within 6 months.
- Chronic ITP: Requires ongoing management, with regular follow-ups to monitor platelet counts and adjust treatment.
Qualitative Platelet Disorders
Qualitative Platelet Disorders occur when platelet count is normal, but their function is impaired, leading to blood clotting problems. These can be congenital or acquired.
Congenital Disorders
- Glanzmann Thrombasthenia: Deficiency of the platelet glycoprotein IIb/IIIa complex.
- Bernard-Soulier Syndrome: Deficiency of the glycoprotein Ib-IX-V complex on the platelet surface.
- Storage Pool Diseases: Deficiencies in alpha or delta granules.
- Other Rare Disorders: Like May-Hegglin Anomaly and Wiskott-Aldrich Syndrome.
Acquired Disorders
- Drug-Induced Platelet Dysfunction: Caused by NSAIDs, aspirin, and other medications.
- Uremia: Chronic kidney disease leading to platelet function impairment.
- Liver Disease: Reduced production of clotting factors and altered platelet function.
- Cardiopulmonary Bypass Surgery: Platelet dysfunction due to mechanical forces during surgery.
Diagnosis and Treatment
- History and Physical Examination: Detailed bleeding history and family history.
- Laboratory Tests: Platelet function tests, blood smear, and electron microscopy.
- Treatment: Avoidance of antiplatelet drugs, desmopressin, platelet transfusions, antifibrinolytic agents, and specific therapies for underlying disorders.
Management and Support
- Regular Monitoring: For bleeding symptoms and platelet function.
- Patient Education: On recognizing symptoms and avoiding situations that may exacerbate bleeding.
- Genetic Counseling: For understanding the risk of transmission to offspring in inherited disorders.
For more detailed information and personalized advice, please consult a healthcare provider specializing in pediatric hematology and immunology.
Common Symptoms:
Symptoms of platelet disorders may include :

Easy or excessive bruising

Prolonged bleeding from minor cuts or injuries

Petechiae (small red or purple spots on the skin),

Nosebleeds

Gum bleeding

Heavy menstrual bleeding
Treatments:
- Corticosteroids to suppress the immune system
- Intravenous immunoglobulin (IVIG) therapy
- Platelet transfusions
- Medications that stimulate platelet production
Frequently Asked Questions
What causes immune thrombocytopenia (ITP)?
ITP occurs when the immune system mistakenly attacks and destroys platelets, leading to a low platelet count. The exact cause is unknown, but it may be triggered by viral infections, medications, autoimmune disorders, or certain cancers.
How is ITP diagnosed?
Diagnosis typically involves a physical examination, blood tests to measure platelet counts and assess platelet function, and may include additional tests such as a bone marrow biopsy to rule out other causes of thrombocytopenia.
What are the treatment options for ITP?
Treatment for ITP aims to increase platelet counts and prevent bleeding complications. Options may include corticosteroids, IVIG therapy, platelet transfusions, medications that suppress the immune system, and in some cases, splenectomy (surgical removal of the spleen).
Is ITP a lifelong condition?
For some individuals, ITP may resolve spontaneously or with treatment, while others may experience chronic or relapsing episodes. Regular monitoring and management by a healthcare professional are essential to optimize outcomes and quality of life.
Can platelet disorders be prevented?
While platelet disorders such as ITP may not be preventable, maintaining a healthy lifestyle, avoiding activities that increase the risk of injury, and seeking prompt medical attention for any unusual bleeding or bruising can help manage symptoms and reduce complications.
Book an Appointment
Important Links
Contacting
Treatments
About Dr. Shraddha
Charity & Welfare
Happy Kids Foundation is a leading Non-Profit Organisation dedicated to help children for weaker socio-econimic backgrounds get the right treatments for Blood-related disorders. To get Involved / Volunteer / Donate, click the button below: